Migraines: Are they being misdiagnosed?

Migraine is one of the World Health Organization’s 20 most disabling conditions. Approximately 12% of the population in the United States have migraines occur, and it is a number that is consistent amongst most western countries.
According to the American Migraine Foundation, a person is said to have migraines “ if within his/her lifetime there have occurred 5 or more attacks of unprovoked headache lasting 4-72 hours, severe enough to markedly restrict or even prohibit routine daily activity and accompanied by nausea or light/ sound sensitivity.” The International Classification of Headache Disorders third edition (ICHD-3) furthers this definition by stating that at least 2 other characteristics, such as unilateral location, pulsating or throbbing, moderate or severe pain, aggravated by or causes avoidance of routine physical activity, are present.
Scientists believe that suffering from migraines runs within families since 80% of sufferers have a first-degree relative who also suffers from migraines. (Headache and Migraine Biology and Management, Ten Things You and Your Patients with Migraine Should Know)Because of the varying conditions with migraines, scientists and doctors fear that they can often be misdiagnosed upon initial visits to hospitals, doctor's offices, and even sleep centers. One disorder that’s often secondary to migraines is migraine mimics.
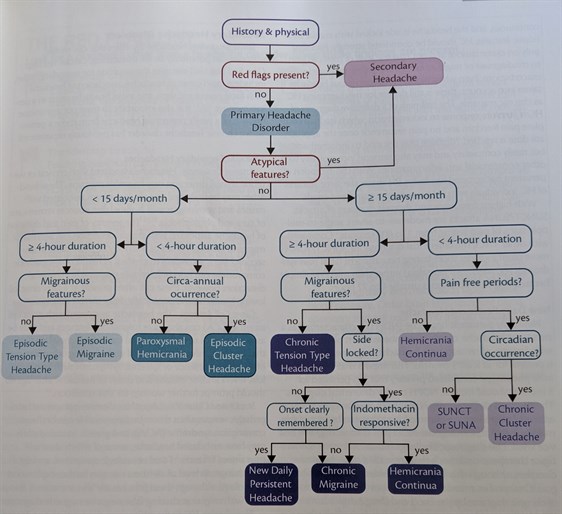
In a recent study by Cynthia E. Armand, Alina Masters-Israilov, and Richard B. Lipton published in Practical Neurology, Volume 18, Number 4, they explore the diagnostic approach of migraines after the initial consultation, which normally leads to a diagnosis in migraine mimics. In the study Armand and colleagues layout a migraine mimics diagnostic algorithm. This algorithm helps doctors determine if patients are suffering from primary headache disorders, like cluster headache, paroxysmal hemicranias, hemicrania continua, and short-lasting unilateral neuralgiform headache attacks with/without conjunctival injection (these primary headaches are grouped together to for Trigeminal Automatic Cephalalgias, or TACs), or secondary headaches, like vascular secondary headaches, cerebrospinal fluid pressure-related secondary headache, headache associated with neoplasms, infectious secondary headaches, toxic and metabolic headaches, and others.. As treatment continues, migraine mimics are still considered depending on the patient’s reaction to treatments.
Practical Neurology, Volume 18, Number 4
Armand et al
Patients who have favorable reactions to treatments may experience exacerbations. When these occur, there are multiple explanations as to why. From outside factors such as life stress, injury, or overuse of medications. Another possibility is that a new type of headache has surfaced. The new headache could be primary or secondary and developed in the setting of the preexisting migraine.
Armand and colleagues came to the conclusion that due to the variety of symptoms and patterns that can express a migraine, it can be extremely difficult to diagnose migraines, especially at an initial visit of a patient. It is often that a false positive or false negative will be the result of the visit. Because of the overlaps that exist in headache qualities and features, it is important that have a thorough history when evaluating those with headaches, and the ability to find features they are experiencing can be paramount in making the right diagnosis. Also, secondary headache disorders can strongly mimic migraines and may be overlooked, which can lead to grave consequences. It is important to remember that a patient can have more than one diagnosis, which can lead to a more expansive treatment process.
“In the end, the answers to our evaluation lie in a comprehensive history and physical exam that should be challenged periodically especially in the absence of improvement despite treatment.” -Armand et al
Cynthia E. Armand, MD
Assistant Professor of Neurology
Albert Einstein College of Medicine
Associate Headache Fellowship Director
Montefiore Headache Center
New York, NY
Alina Masters-Israilov, MD
Fellow, Headache and Facial Pain
Department of Neurology
Montefiore Headache Center
New York, NY
Richard B. Lipton, MD
Edwin S. Lowe Professor and Vice Chair of Neurology
Professor of Epidemiology and Population Health
Professor of Psychiatry and Behavioral Science
Director, Division of Cognitive Aging and Dementia
Director, Montefiore Headache Center
Albert Einstein College of Medicine
New York, NY
